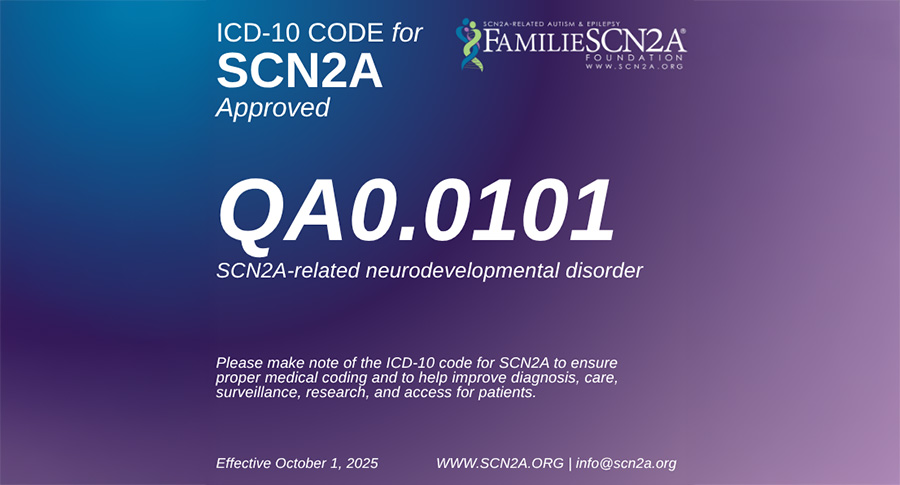
The FamilieSCN2A Foundation is thrilled to announce that advocacy efforts with the CDC over the last four years have resulted in the assignment of a unique ICD-10-CM code for the SCN2A community. Effective October 1, 2025, the new code for SCN2A-related neurodevelopmental disorders will be QA0.0101.
“An ICD-10-CM code for SCN2A means that clinical care data on anyone with an SCN2A- related disorder can now be tracked using this specific code. This will translate to improvements in research methods and clinical care for our community. It’s a huge win. Now we need everyone to encourage all their healthcare providers to use it, to ensure the code represents the SCN2A community to clinicians, insurers, the FDA, and researchers as accurately and completely as possible,” said Leah Myers, Executive Director of FamilieSCN2A Foundation.
Long Process to Get the New Code
The FamilieSCN2A Foundation first applied for the ICD-10-CM code in June, 2021, and have worked closely with the CDC to help make a case for why it was so important to include this community in the classification system.
“The ICD-10CM code was a massive undertaking. Our community, including patient advocates, research scientists, and clinicians, worked with the CDC for four years to get SCN2A-related disorders recognized with its own code - a huge step toward making sure that health care providers, payors, industry and the FDA recognize SCN2A. We are profoundly grateful to the efforts of Scott Demarest, MD, Children’s Hospital of Colorado, who initially presented SCN2A clinical features, clinical care procedures, and natural history to the CDC. Key opinion leaders and dedicated clinicians were rallied by FamilieSCN2A Foundation’s leadership board (Eloise Austin, Leah Myers, and Jenny Burke) to individually write hundreds of letters of support advocating for SCN2A-related disorders to be recognized in this manner,” said Shawn Egan, PhD, Dad of Harper and Chief Scientific Officer of FamilieSCN2A Foundation who led these efforts. “We’d also like to thank the CDC's National Center for Health Statistics (NCHS) and the World Health Organization (WHO), which owns and publishes ICD-10, for assigning this code and coordinating its global use throughout the world.”
What are ICD-10-CM codes:
When a person gets medical care, their health conditions and symptoms are listed in their medical record using International Classification of Diseases (ICD) codes. These codes are used all over the world to help document conditions in a standard way that allows for robust analysis for many purposes. (Note: The use of data from ICD codes is HIPAA compliant.)
While there are tens of thousands of highly-specific ICD-10 codes, many rare disorders like SCN2A-related disorders don’t have their own code and are lumped into generic categories. Without a unique code, it can be nearly impossible to use healthcare databases to find out information about a specific community of individuals like those living with SCN2A-related disorders.
ICD codes are used for many purposes, including healthcare billing, research, public health surveillance, drug development, and advocacy efforts. Some examples for how the SCN2A community may benefit from having a unique ICD-10 code:
• ICD-10-CM codes directly impact healthcare: Many electronic medical record systems incorporate ICD-10 codes to provide clinicians with treatment guidelines, decision-making tools, and automated alerts regarding best practices for the condition
• Healthcare providers can track what treatments, services, and conditions (or co-morbidities) are more likely to occur in people with SCN2A-related disorders. This knowledge can help with planning and prevention.
• Researchers can learn more about how and when early symptoms develop in people later diagnosed with SCN2A-related disorders. This can help healthcare providers identify at-risk people earlier and improve outcomes by reducing delay in treatments.
• Healthcare payers can understand the cost of long-term care of a person with SCN2A-related disorders. They can compare conventional symptom management (including hospitalizations, rehabilitative services, etc.) vs. the cost of paying for an expensive new treatment option such as ASO therapy or gene therapy. Understanding the true cost of care may help increase the likelihood of coverage for disease modifying treatments.
• Public health organizations can get a better sense of the number of individuals who are affected by SCN2A-related disorders, helping to improve incidence and prevalence statistics. Using ICD-10 data can help count everyone who has been diagnosed, even if those people do not participate in patient registries, research projects, clinical trials, or other efforts to gather data.
• Drug developers and regulators (like FDA) can get a better understanding of the natural history of SCN2A-related disorders. This information can be very helpful in demonstrating unmet needs, designing meaningful clinical trials, and providing data to support biomarker development.
• Advocacy leaders like The FamilieSCN2A Foundation can learn more about symptoms, related conditions, and healthcare usage of people they represent. This can lead to better outreach, advocacy plans, and collaborations with partnering organizations.
Using the New ICD-10 Code
It’s important to note that the SCN2A code (QA0.0101) is not meant to replace other condition codes; rather, it is used in addition to other codes for related disorders (such as autism or epilepsy). Some of these other conditions may be known manifestations of SCN2A genetic changes, and others might be unrelated conditions like allergies.
For example, someone with SCN2A-related epilepsy might have several codes in their chart, including:
QA0.0101 - SCN2A-related neurodevelopmental disorder
R56.9 - Seizure
Z99.3 - Dependence on wheelchair / wheelchair as ambulatory aid
J30.81 - Allergic rhinitis due to animal (cat) (dog) hair and dander
Someone with SCN2A-related autism might have a chart that looks like this:
QA0.0101 - SCN2A-related neurodevelopmental disorder
F84.0 - Autism
M41.9 - Scoliosis
J45.4 - Persistent asthma, moderate
Projects are underway to:
• Identify blood-based biomarkers for IS.
• Develop novel therapeutic options.
• Prevent IS in at-risk populations.
Families are encouraged to share the new code with all healthcare providers, including primary care, specialists, and urgent/emergency care providers. In the upcoming months, the FamilieSCN2A Foundation will take the lead in providing education and promotion materials to families and clinicians.
To watch a recorded Townhall Meeting that discussed the SCN2A ICD-10 code on June 20, 2025, click here: https://youtu.be/NJhi4cCiLcg
#ICD10Code #BigWin #ClinicalCare
Frequently Asked Questions
Drugs typically have to clear multiple clinical trial hurdles in order to support approval. The typical trial phases are 1, 2, and 3 with lower number being earlier trials and larger numbers being more advanced trials.
Phase 1 trials are typically in healthy volunteers and are evaluating initial safety, and dosing in humans. These trials help ensure that the drug is safe enough to be evaluated in patients and also are used to identify an appropriate dosing range for subsequent trials.
Phase 2 trials are typically used to provide proof of concept (that the drug has an efficacy signal, is providing a benefit to patients) and also tests safety in the patient population. These trials often are used to help design and power registrational phase 3 trials.
Phase 3 trials are often the trials used to support the approval of the agent and may be the final clinical hurdle a drug needs to pass in order to be approved by the FDA.
This is a designation granted by the FDA when a drug is being developed to treat a pediatric condition that is serious and life-threatening and occurs in under 200k people in the US.
This is a program used by the US government to incentivize drug development for pediatric rare diseases. If a drug is approved that has been granted the rare pediatric disease designation, then the developing company receives a voucher that grants priority review of a future drug (which can accelerate the developmental time of a drug by ~4 months; for example: if drug#1 is approved and had been granted the rare pediatric disease designation then said company would receive a priority review voucher that they could use on drug#2 ).
This is a designation granted by the FDA when a drug is being developed to treat a rare disease (occurs in under 200k people in the US).
This is a program used by the US government to incentivize drug development for rare diseases. Drugs awarded this designation received a number of incentives by the FDA including: 1. Market exclusivity for 7 years post approval, 2. A waiver of application of user-fees, and 3. A 50% tax credit for clinical testing expenses